COVID-19 swept through the world like a hurricane, leaving destruction in its wake and changing the world entirely. From masks in shops to hand sanitizers at every turn – there are practices in place that we once didn’t have to deal with. Perhaps the most profoundly affected industry is healthcare – an industry forced to rapidly adapt so that it can keep patients and staff safe. Has it been easy? No. But it opened doors to better sanitation practices and policies that hospitals may have needed long before COVID-19 struck.
Nevertheless, they’re here, and they’re here to stay for the foreseeable future, so let us explore what they are.
Hand Sanitization and Masks
Hand sanitization and mask-wearing are two of the most overbearing sanitization change healthcare experienced. It affected staff, patients, and visitors. Staff must wear a standard face covering when entering the hospital, and for certain patient encounters, such as entering a room where someone is COVID-19 positive – the mask changes to an FFP3. FFP3 masks are tight-fitting to prevent the inhalation of airborne droplets.
Hand sanitization was somewhat a given in hospitals – it’s nothing new. But the policing of it is. Staff are encouraged to make visitors sanitize their hands before entering a clinical area and when leaving. The familiar hand gel devices have always been in hospitals – they’re just now clearer to see and easier to use, with many hospitals investing in automatically dispensed hand gel to prevent infection spread.
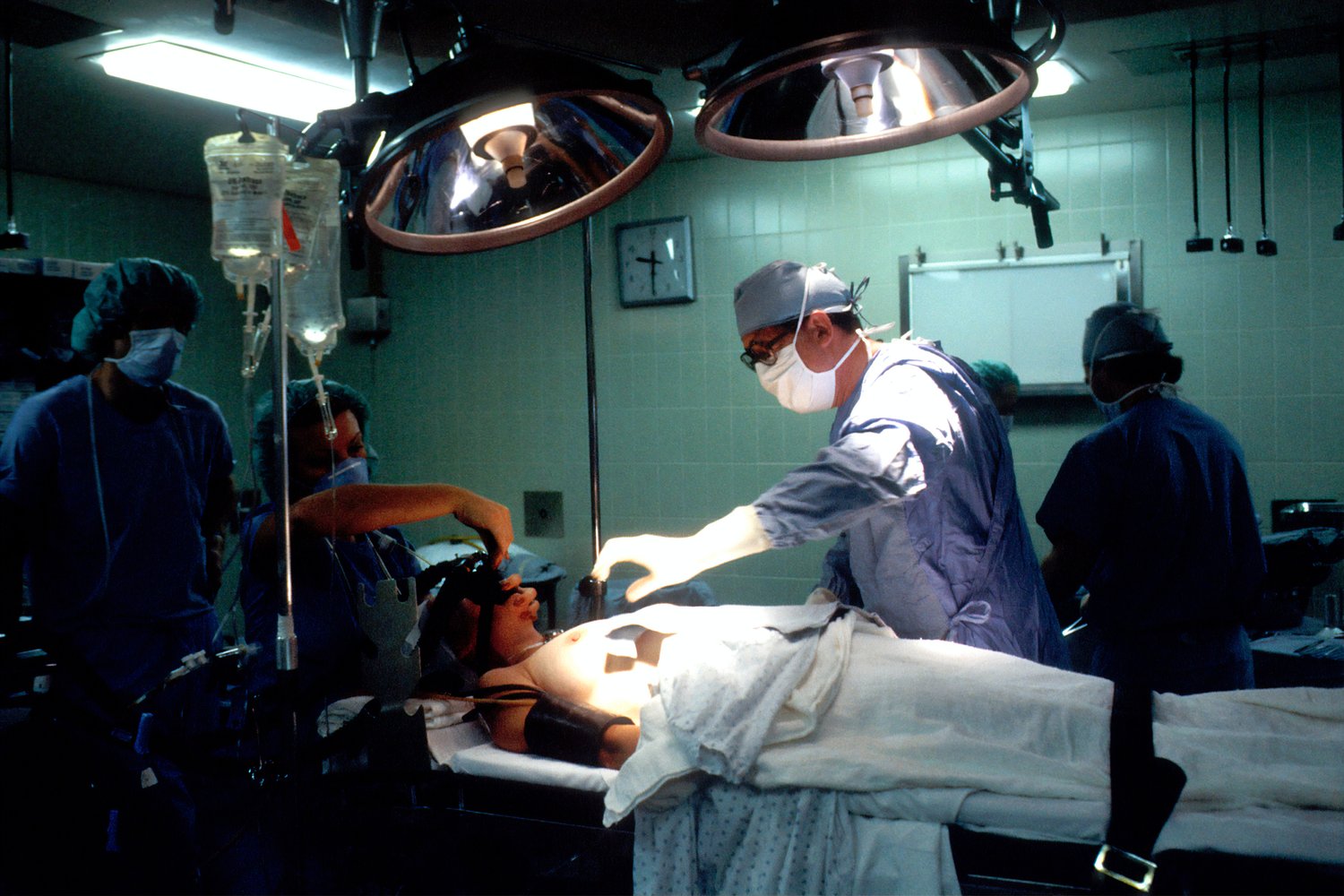
Stringent Surgical Changes
Theatres have experienced the strictest changes because most operations, especially ones involving anesthesia, involve aerosol-generating procedures. Aerosol-generating procedures have the potential to disperse airborne droplets throughout the operating room, which increases the risk of COVID-19 infection transmission.
For that reason, hospitals require patients to have a negative COVID state. For ones that don’t, there are what’s known as ‘dirty’ operating rooms where the strictest infection prevention guidelines for COVID-19 must be followed.
Other changes involve the equipment and how it’s used and cleaned. One example is the surgical retractor – there’s now the option for a single-use plastic device to be selected over the old metal retractor. It aims to reduce the spread of infection and make surgical procedures simpler. Take a look at the self-retaining retractor, innovated with surgical grade plastic, here https://junemedical.com/galaxy-ii-overview/surgical-retractors-info/.
PPE Rules
PPE is something we’ve all heard of, but it stands for personal protective equipment. Guidelines on its use have changed – but all staff must now wear PPE — including mask, gloves, and apron — for all patient contacts. When entering a room with a patient with confirmed COVID-19, it’s a mask, apron, gloves, visor, and gown. The changes aim to protect both staff and patients and minimize the risk of transmission throughout the ward.
There was once a time when staff members would have to wear visors 24/7, but this is now limited to contact with COVID-19 positive patients only.
COVID-19 is still wreaking havoc globally and still requires the world of healthcare to evolve and change practices. With the announcement of new variants and vaccinations failing – it seems COVID-19 isn’t finished with healthcare just yet.